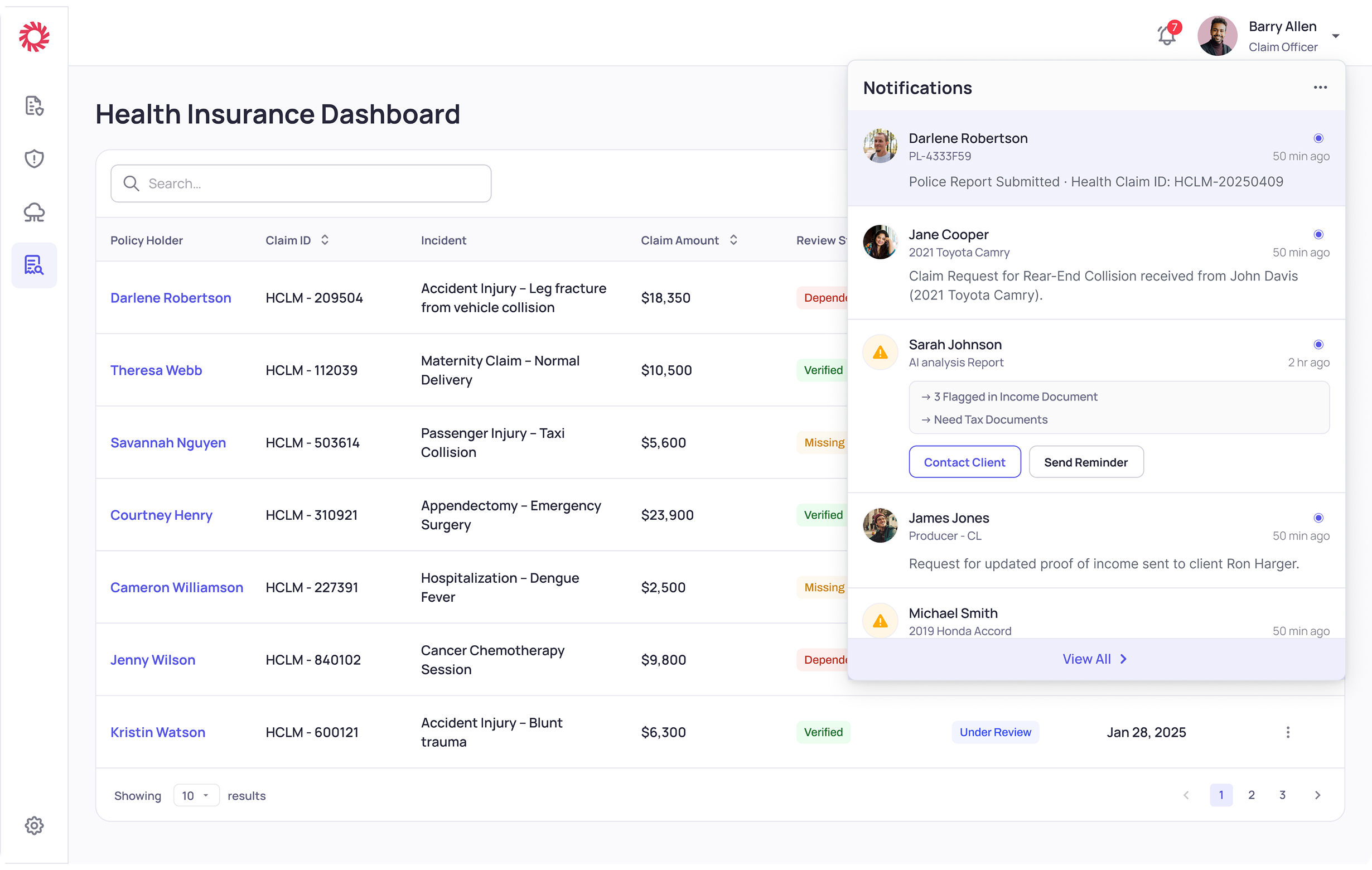
Client Overview
A seasoned Caribbean insurance leader, with 700+ professionals and 30 years of expertise, provides comprehensive coverage. Their portfolio spans health, automobile, and a wide array of pension solutions.
Since implementing hyper-automation, we've observed significant improvements in operational efficiency and data quality:
Since implementing hyper-automation, we've observed significant improvements in operational efficiency and data quality:
30%
Increase in customer interactions within 3 months, indicating enhanced engagement.
5,000+
Hours Saved annually, showcasing optimized operations.
95%
Data Accuracy achieved, ensuring superior data integrity.